Can regenerative medicine change how we treat Peripheral Arterial Disease (PAD)? This disease affects over 10 million in the U.S. Many believe stem cell therapy is a new hope for the pain and risk of amputation in severe cases.1 It focuses on growing new blood vessels and restoring blood flow.
This could be a big step away from the usual surgeries for PAD. These surgeries are often risky and some patients can’t have them.1 Studies are showing how this new method might be the answer we’ve been looking for in managing vascular health.

Key Takeaways
- Peripheral arterial disease (PAD) affects more than 10 million people in the United States.1
- PAD is characterized by the narrowing of blood vessels in the limbs due to fatty plaque build-up.1
- Regenerative stem cell treatment aims to regenerate new vessels and restore blood flow.2
- The existing methods like angioplasty and bypass surgery may not be suitable for all PAD patients.1
- Stem cell therapy represents a significant shift towards more effective management of PAD.1
Introduction to Peripheral Arterial Disease (PAD)
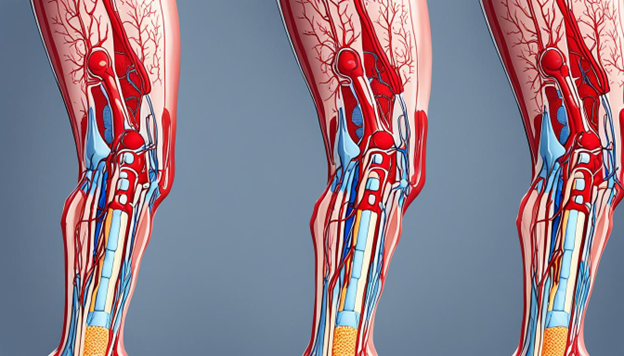
Peripheral Arterial Disease (PAD) affects the blood circulation in the body. It narrows the arteries, reducing the flow of blood to the limbs. This leads to serious problems such as leg pain while walking and difficulties in healing wounds.
The main cause is when fatty plaque builds up in the arteries. This mostly happens in people in middle-age or older. If someone smokes, has diabetes, high blood pressure, or high cholesterol, they’re at a higher risk for PAD.
Lifestyle choices and other health problems make it worse. For example, having diabetes can make someone more likely to get PAD3. Studies also show that people with PAD and other health issues might not get better with some treatments3.
There’s more PAD in African American and Hispanic people. This shows genetics and lifestyle are big factors too4. It’s why we need special efforts to fight PAD in these groups.
We must understand PAD and its risks to help those with it. Knowing the right ways to care for it can make a big difference for patients, especially those at more risk.
Current Treatment Options for PAD
The management of Peripheral Arterial Disease (PAD) mainly uses surgeries like angioplasty and bypass operations. These help get rid of blockages or create new paths for blood flow. These surgeries are effective but also carry risks. For example, in a 2020 study in the New England Journal of Medicine, mortality rates related to paclitaxel-coated devices were concerning4. Also, there’s a high risk for patients with visible signs of PAD4.
But for some patients, like those with severe PAD or no good veins for surgery, options are scarce. Critical limb ischemia (CLI), a dangerous complication, is a big challenge affecting many5. This urgent need for new treatments stresses the importance of stem cell therapy as it aims to grow new blood vessels. This improves blood circulation in the limbs that are suffering5.

New developments in regenerative medicine are quite significant. A large number of cases with CLI underscore the widespread impact5. Now, many are researching the potential of using a patient’s own stem cells for treatment5. Assessing vascular health and using new regenerative methods could fill the gaps in current treatments. This change is crucial due to the need shown in patient data and practical experiences5.
Overall, even though surgeries are a common treatment for PAD, their limitations mean we must explore new options like stem cell therapy and improved surgeries. This forward-thinking is key for offering better care to those with PAD.
What is Regenerative Medicine?
Regenerative medicine works on fixing or replacing damaged tissues and organs. It uses stem cells to kickstart the body’s own healing. This is vital for cases where usual treatments don’t work.
Understanding Regenerative Medicine
Regenerative medicine mainly uses stem cells. These cells can become many different types, helping repair the harm caused by diseases or injuries. They bring fresh hope for people with issues like peripheral arterial disease (PAD)1. This disease affects millions in the U.S.
Benefits of Regenerative Medicine
It has several benefits, especially for vascular issues such as PAD. It provides options besides surgery, boosting life quality. The use of nanofibrillar scaffolds has led to better blood flow in affected areas1. Also, stem cells grow faster with these scaffolds, showing the huge promise of this therapy1.
Using regenerative medicine in medical settings can help with endothelial dysfunction. This is a significant issue in PAD’s development6. Therapies like therapeutic angiogenesis and stem cell transplants look very promising for PAD management6.”
Stem Cell Therapy: A New Approach to PAD
Peripheral arterial disease (PAD) hits millions in the US. Some have it so bad that regular surgery won’t help1. But, stem cell therapy steps in as a new hope. It works to grow new vessels and bring back blood flow. This way, it tackles PAD at its core, opening doors to a brighter life.
How Stem Cells Work in Regenerative Medicine
Stem cells are key in regenerative medicine. Their job is to turn into different cell types. This makes them great for fixing up tissues in PAD. They let off growth factors that help make new blood vessels. As a result, blood flow and tissue healing get better2.
Around the world, research shows that adding nanofibrillar scaffolds to stem cells makes a big difference. It boosts the growth factors they produce way more than just using saline1. This boost can help the body heal better on its own, showing stem cell therapy can really work for PAD patients.
Types of Stem Cells Used in PAD Treatment
There are different stem cells for PAD, each with special powers. For example, stem cells from human fat are great because they can turn into lots of cell types2. This has been proven time and again by researchers2.
Then, there are mesenchymal stem cells, taken from either bone or fat, which are also quite something. They can calm down the immune system and even become the cells that line blood vessels. This makes them top-notch for pushing vascular health and bringing back blood flow in PAD folks.
Stem Cell Treatment Peripheral Arterial Disease
Stem cell treatment for peripheral arterial disease (PAD) is a cutting-edge method that injects stem cells into the affected limbs. This aims to repair damaged blood vessels and improve blood flow. It offers new hope for patients with blocked arteries and severe PAD, especially when traditional methods have not been very successful. According to Criqui et al. (1985)2, around 71% of certain areas’ populations are affected by this disease. Also, a study from the National Health and Nutrition Examination Survey showed a 4.3% PAD prevalence in the U.S. from 1999-20002.
Stem cell injections introduce mesenchymal stem cells. These cells can help control immune reactions and encourage the regrowth of tissues2. Experts often perform these injections in clinics focused on treating PAD. A 2008 study in Vascular Medicine found that special biomarkers can track how well these treatments are working6.
Studies show the exciting potential of using stem cells to treat blocked arteries. For example, the ACC/AHA 2005 Practice Guidelines stress the importance of various groups working together to tackle PAD6. In addition, early studies on transplanting a patient’s own bone marrow cells have shown good results for treating limb ischemia6.
As research progresses, the safety and effectiveness of these treatments become clearer. An international study by Deev et al. showed positive results in 210 PAD patients2. Also, using a patient’s own bone marrow cells repeatedly has proven beneficial over time. This approach is offering a new path for managing chronic limb ischemia and foot ulcers better6. The world of regenerative medicine is advanced and ever-changing. Stem cell approaches for PAD offer hope for better outcomes for patients.
Recent Studies and Breakthroughs
New discoveries in using stem cells for peripheral artery disease have brought big advances. These findings have helped improve how we treat patients. They’ve also shown us more of what this treatment can do.
Notable Research Findings
A meta-analysis in 2019 by Song et al. showed that many in China have peripheral artery disease. This was big news. It means we need to find better ways to help these patients4.
Then, in 2017, Hiatt et al. found that ticagrelor works better than clopidogrel for these patients4. This is important for doctors to know when choosing treatments. Another key point came from Bonaca et al.’s 2020 study. They showed that rivaroxaban helps patients after they’ve had surgery4.
Case Studies and Patient Outcomes
Success stories in PAD research show us a lot. For example, Xie B et al.’s work from 2018 proved that a certain stem cell therapy can really help patients. This led to new and better ways to treat them5.
In 2012, Losordo DW et al. studied another type of stem cell therapy. It focused on using the patient’s own CD34+ cells to treat severe cases. This approach was very effective5.
All this recent work shows us the amazing potential of stem cell treatments for PAD.
Challenges and Limitations
Stem cell therapy shows great promise for treating PAD but it also faces big hurdles. A key issue is the survival of stem cells right after being transplanted1. Using nanofibrillar scaffolds and getting stem cells to live in low-oxygen areas can help, as they promote new blood vessel growth1.
Patients may respond differently to stem cell treatment for PAD. For some with PAD, high levels of certain inflammation markers might mean the therapy won’t work well3. The success of the treatment also varies because of differences in genes and blood levels3. So, it’s hard to know ahead of time who will respond best to the therapy.
To apply stem cell therapy on a broad scale, we must tackle many challenges. Making the process of collecting, growing, and giving stem cells standard and safe is key. Working through these problems is crucial for making stem cell therapy widely available for PAD treatment. Improving how we deal with these issues is vital for better cell-based therapies3.
Future of Stem Cell Therapy for PAD
The future of stem cell therapy for PAD looks bright. Ongoing research is improving how stem cells are delivered and how well they survive. Scientists are looking into using nanofibrillar scaffolds. These could help stem cells work better once inside the body.
Ongoing Research and Innovations
Researchers are trying out new ways to make stem cell therapy work better for PAD. They are looking into personalized medicine. This approach tailors treatments to meet each patient’s specific needs. It could make treatments more effective. Successful revascularization has also shown that improving how procedures are done can really help PAD patients4.
Predicted Advancements and Their Impacts
Experts believe there will be big changes in treating PAD in the future. One exciting development is the use of dual-antiplatelet therapies. They have the potential to decrease serious heart events in PAD patients4. Adding statin therapy after initial revascularization is expected to boost outcomes too4. Moreover, new delivery methods using nanotechnology might make stem cells even more powerful7.
| Advancement | Impact |
| Nanofibrillar Scaffolds | Improved stem cell integration and effectiveness |
| Personalized Medicine | More targeted and effective interventions |
| Dual-antiplatelet Therapies | Reduced major adverse cardiovascular events4 |
| Statin Therapy | Enhanced clinical outcomes post revascularization4 |
| Advanced Delivery Methods | Increased stem cell survival and functionality7 |
Conclusion
The use of stem cell therapy could change how we treat peripheral arterial disease (PAD). It affects about 12.9% of people in the U.S. PAD is a severe issue, needing new treatments fast.2 Stem cell therapy works by creating new blood vessels. This helps improve blood flow, which is key for good vascular health.
This new method has shown real promise. For example, stem cells from fat can yield 7 to 14 cells from every 100 mm³ of fat removed during liposuction. This indicates we can get a lot of cells for treatment.2 Also, studies show mesenchymal stem cells can change how immune cells respond. This boosts their healing effects.2 These positive results hint that the future PAD treatments could be more powerful and less risky.
A team effort is crucial in treating PAD with stem cell therapy. Combining traditional medicine and stem cells can help patients live longer. It shows the power of mixing old and new treatments well.8 More research and development promise exciting new ways to care for PAD patients. It brings hope for a better life quality.
FAQ
What is Peripheral Arterial Disease (PAD)?
Peripheral Arterial Disease (PAD) is a common issue. It makes arteries in the body narrow. This slows down blood flow to the legs. The result is pain and problems moving the legs. Often, atherosclerosis causes PAD.
What are the symptoms of PAD?
Signs of PAD include leg pain when walking or resting, cramps, and weakness. In worse cases, you might see wounds that don’t heal or might need to have a limb removed.
What are the risk factors for developing PAD?
Things that increase your risk for PAD are smoking, diabetes, and high blood pressure. Having high cholesterol and getting older are also factors. PAD is more common in African American and Hispanic groups.
What are the current treatment options for PAD?
Doctors treat PAD with lifestyle changes, drugs, and surgeries. Treatments like angioplasty and bypass surgery help. But, for severe cases with no good vessels for surgery, choices are few.
What is regenerative medicine?
Regenerative medicine aims to fix, renew, or replace damaged parts of the body. It often uses stem cells.
What are the benefits of regenerative medicine?
It can help the body heal damaged tissues and work better again. Especially when other treatments don’t work.
How does stem cell therapy work in regenerative medicine?
Stem cells help repair and regenerate tissues. In PAD, they enhance blood flow by growing new blood vessels.
What types of stem cells are used in PAD treatment?
Mesenchymal stem cells are common for PAD. They come from bone marrow or fat.
How are stem cell treatments administered for PAD?
Doctors usually inject stem cells into the legs. This helps grow new vessels and improve blood flow.
What recent studies and breakthroughs have been made in stem cell therapy for PAD?
Recent research on stem cell use for PAD looks good. It points to better blood flow in legs and lower amputation risk. More studies confirm these treatment benefits.
What are the challenges and limitations of stem cell therapy for PAD?
Making sure the stem cells survive and reach the right places is hard. But, solving these issues would make the treatment better.
What is the future of stem cell therapy for PAD?
Researchers are working on better ways to use stem cells for PAD. If they succeed, it could change how PAD is treated for better.
Source Links
- https://med.stanford.edu/cvi/mission/news_center/articles_announcements/an-improved-stem-cell-based-treatment-for-peripheral-arterial-disease.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6539394/
- https://www.mdpi.com/2073-4409/10/12/3266
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10278215/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10416751/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3846073/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8699290/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6528204/