Erectile dysfunction (ED) is a common condition in men where they have difficulty getting or maintaining an erection for satisfactory sexual intercourse. It affects almost 1 in 5 men aged 20 years or older, and the prevalence is even higher in older men.
Erectile dysfunction can affect a person’s overall wellbeing and quality of life, leading to depression, anxiety, relationship issues, and feelings of inadequacy. ED can also indicate existing health conditions such as vascular disease or diabetes, as well as issues with blood flow. In some cases, it may be an indicator of hormonal abnormalities or cardiovascular disease.
Doctors often prescribe medications called phosphodiesterase type 5 inhibitors (PDE5Is) to treat ED, which are usually safe and effective. However, up to 1 in 3 patients with ED may not respond well to these medications. This is especially true for those who have had pelvic surgeries or have diabetes, as these conditions can reduce the amount of a chemical called nitric oxide that is needed for the medications to work.
Thankfully, there is ongoing research to find other treatments for ED. Some studies have found that certain types of regenerative cells, both cultured and uncultured, can restore erectile function in animal models of nerve injury and diabetes. Some human clinical trials have been conducted using these regenerative cells to treat ED, with promising results.
However, there are some challenges to using these regenerative cells. Uncultured cells are not as convenient because they cannot be stored for multiple injections. Cultured cells, such as stem cells, may be more effective, but there is a risk of the body’s immune system reacting to them if they are repeatedly administered.
A study, Safety of autologous bone marrow-derived mesenchymal stem cells in erectile dysfunction: an open-label phase 1 clinical trial, looked into the safety and potential of stem cell therapy for patients with ED.

Results of the Study
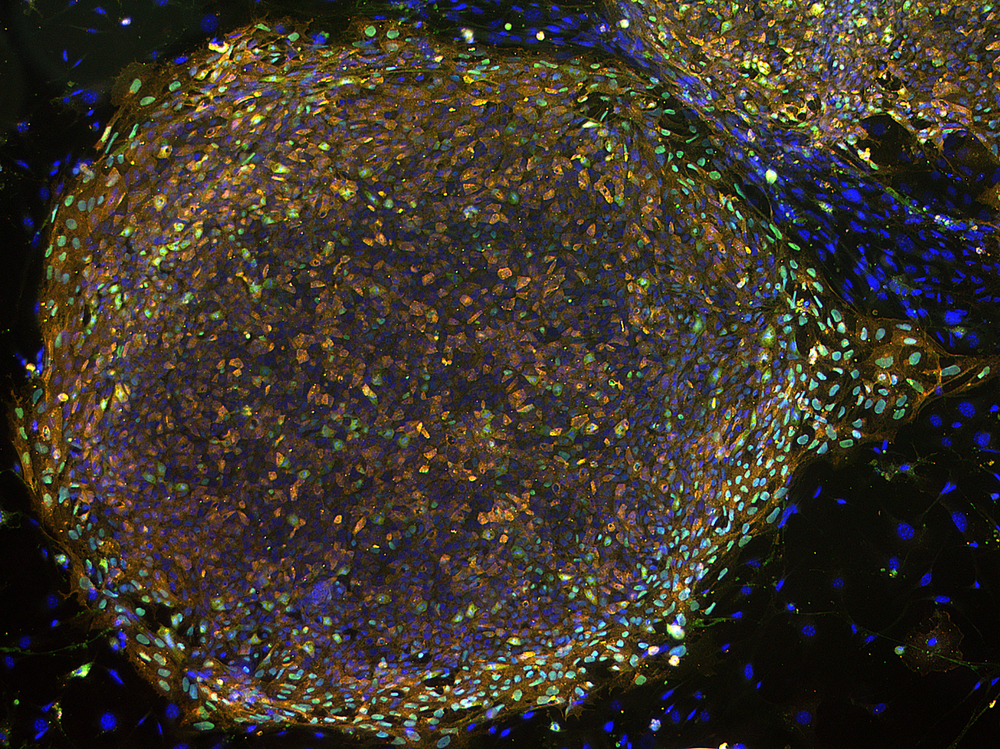
Out of 13 patients who were screened, 10 were able to join the clinical trial and received a treatment called bone marrow-derived mesenchymal stem cells (BMSCs). Nine patients finished the trial. Bone marrow-derived mesenchymal stem cells were taken from the patients’ own bone marrow and injected into the penis once, one month after the cells were collected. The patients were monitored for safety and effectiveness at various points over the course of a year.
To prepare for the injection, the BMSCs were harvested and washed. They were then mixed with a solution and put into a syringe. A tourniquet was used to help the injection spread evenly throughout the penis, and the patients were monitored for any side effects for at least two hours after the injection.
The main goal of the trial was to look for any side effects that might have been caused by the treatment. The patients were also monitored for changes in their erectile function using a questionnaire and other tests. The researchers looked for any abnormal lab results, vital signs, and physical exam findings that could be linked to the treatment. The safety and efficacy of this treatment was monitored with follow-up hospital visits at 1, 3, 6, 9 and 12 months post-injection.
The researchers also wanted to see how well the treatment worked. The patients’ erectile function was assessed using a questionnaire, and other tests were done to evaluate the results. The patients were asked to rate their sexual function and satisfaction with the treatment. Penile Doppler sonography was also used to measure blood flow in the penis.
During the clinical trial, some patients experienced side effects, but they were mild and not related to the treatment. There were no serious side effects, and no one dropped out of the trial because of side effects.
The patients were monitored for changes in their erectile function using a questionnaire and other tests. One month after the treatment, the patients’ erectile function improved significantly, but the improvement was not significant at other times during the year-long study. Other tests were done to evaluate the results, including measuring blood flow in the penis. However, there were no significant changes in blood flow during the study.
While the results of this study did not show significant improvement in erectile function beyond the first month after treatment, the side effects were mild and there were no serious complications. The phase 1 clinical trial showed that autologous BMSC therapy for erectile dysfunction is safe and did not cause any side effects. This is good news for patients with ED who are looking for safe and effective treatments. However, more studies are needed to confirm the effectiveness of this treatment in larger groups of patients, in randomized, placebo-controlled clinical trials.