Ankylosing spondylitis (AS) is a painful and difficult to manage chronic inflammatory condition of the axial skeleton, peripheral joints, and nonarticular areas. Ankylosing spondylitis can have a major impact on patients’ quality of life. Chronic pain, joint stiffness and fatigue characterize the condition, making it difficult to participate in typical activities of daily living.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to help reduce pain and inflammation in AS patients. While they can be effective, they may cause unpleasant side effects such as gastrointestinal and cardiovascular toxicity in some patients. Additionally, research has shown that sulfasalazine was not found to be beneficial in the majority of cases. Conventional disease-modifying antirheumatic drug treatments have had limited success for those suffering with peripheral joint disease as well.
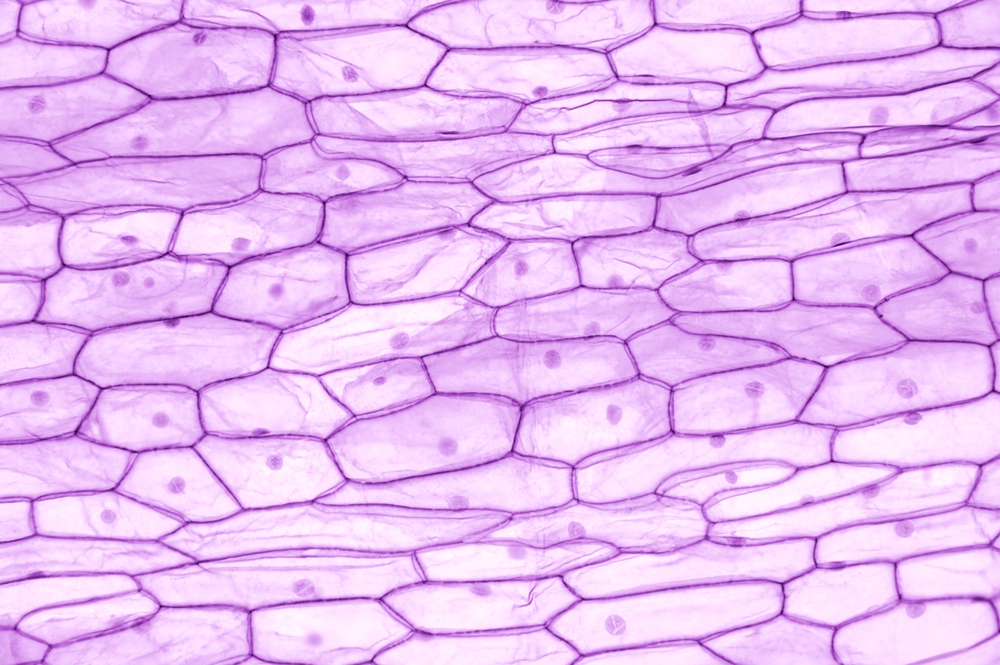
Recent studies have shown that AS is an autoimmune disease, which means that the body’s immune system is attacking itself. Mesenchymal stem cells (MSCs) are cells that can help regulate the immune system and reduce inflammation. Researchers have found that MSCs can be used to treat autoimmune and inflammatory diseases, such as Crohn’s disease and multiple sclerosis.
While more research is needed, using MSCs to treat AS shows promise as a safe and effective alternative to traditional treatments. By understanding how AS affects the body, researchers are discovering new ways to manage this chronic condition and improve the lives of those affected by it. In a clinical trial, Effects and Safety of Allogeneic Mesenchymal Stem Cell Intravenous Infusion in Active Ankylosing Spondylitis Patients Who Failed NSAIDs: A 20-Week Clinical Trial, researchers looked into the potential of stem cell therapy for AS patients.
The researchers wanted to find a safe and effective way to treat patients with ankylosing spondylitis who cannot take nonsteroidal anti-inflammatory drugs or have not responded to them. They decided to try using mesenchymal stem cells to see if they could help improve patient outcomes.
Results of the Study
The 31 patients in the study received four IV infusions of MSCs over the course of four weeks. The patients received 1 million MSCs per kg body weight in 10 ml solution at baseline, first week, second week, and third week.
The primary efficacy endpoint was to determine the percentage of ASAS20 responders at the fourth week. ASAS20 response is defined as an improvement of more than 20% and at least one unit on a 0-10 cm VAS compared to baseline in at least three out of four domains (patient global, back pain, BASFI, spinal inflammation). Additionally, there must be no worsening by more than 20% or at least one unit in the remaining domain.
The secondary efficacy endpoint measured was the mean duration of ASAS20 response which is calculated by subtracting when ASAS20 response ended from when it emerged for every patient and then dividing it by the number of patients in the final cohort. Other metrics used to assess clinical effects included ASDAS-CRP, BASFI, BASMI, MASES, TBP, PG levels, ESR and CRP levels. All assessments were conducted professionally by trained researchers using proper equipment.
The study found that 77.4% of the patients responded well to the MSC treatment and experienced improvements in their symptoms. The response was measured at various time points after the infusion, with the highest percentage of patients responding at the third week. The improvements lasted for an average of 7.1 weeks.
The study also looked at other factors, such as inflammation levels and spinal mobility. The results showed that the inflammation levels decreased significantly after the MSC treatment, while the spinal mobility improved. The secondary evaluation showed a significant decrease in mean ASDAS-CRP score (which indicates disease activity) from baseline to 4th week with an eventual increase afterwards.
Assessment of BASFI (measuring functional improvement) and BASMI (measuring spinal mobility) also found similar decreases in value along with a decrease in TIE levels post infusion which indicate an overall reduction in inflammation area and intensity across patients. The researchers used MRI to look at the inflammation in the spine and found that it decreased over time. Although the decrease was not statistically significant at the fourth week, it was statistically significant at the 20th week.
Overall, the study showed that MSC infusion could be a safe and effective alternative for people with AS who have not found relief from traditional treatments. By understanding how AS affects the body, researchers are discovering new ways to manage this chronic condition and improve the lives of those affected by it.
The study has some limitations, including the small number of patients involved and the fact that it was not a randomized controlled trial. However, the results are promising and suggest that MSC infusion is a safe and effective treatment for AS.